Living with diabetes creates unique challenges for your oral health, particularly when it comes to gum disease and dental implant treatment outcomes. The relationship between blood sugar control and periodontal health is so strong that diabetes and gum disease often worsen each other, creating a cycle where poor blood sugar control leads to more severe gum problems, which then make diabetes management more difficult.
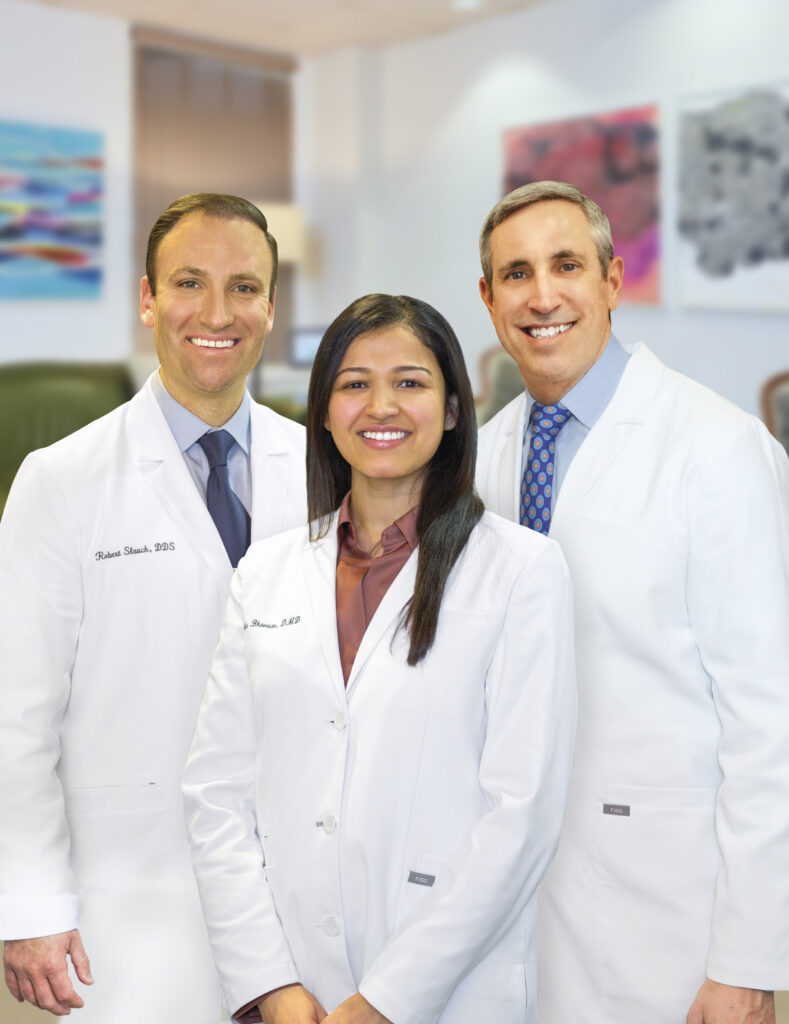
Our Philadelphia periodontal practice understands the complex relationship between diabetes, gum health, and implant success. With more than 49 years of experience treating patients with various medical conditions, we provide comprehensive care designed to help diabetic patients achieve optimal oral health and successful implant outcomes through careful planning, advanced treatments, and ongoing monitoring.
The Diabetes-Gum Disease Connection
Periodontal disease affects nearly 22% of all people with Type I and Type II diabetes, making it the most common dental concern for diabetic patients. High blood sugar levels create an environment where harmful bacteria thrive in your mouth, leading to more aggressive gum infections and faster progression of periodontal disease.
Diabetes impairs your immune system’s ability to fight bacterial infections, including those in your gums. When blood sugar levels remain elevated, white blood cells become less effective at combating the bacteria causing gum disease. This reduced immune response means infections develop more quickly and become more severe than in non-diabetic patients.
The inflammation caused by gum disease also makes blood sugar control more challenging. Periodontal infections trigger inflammatory responses throughout your body, making insulin less effective and causing blood sugar levels to spike. This creates a dangerous cycle where gum disease worsens diabetes control, and poor diabetes control accelerates gum disease progression.
Blood Sugar Control and Healing
Successful periodontal treatment and dental implant outcomes depend heavily on achieving stable blood sugar control before and during treatment. When HbA1c levels remain above 7%, healing becomes significantly slower and complications increase dramatically. Well-controlled diabetes, with HbA1c levels below 7%, allows for much better treatment outcomes.
Poor blood sugar control affects wound healing at the cellular level. High glucose levels interfere with collagen synthesis, reduce blood flow to healing tissues, and impair the formation of new blood vessels needed for recovery. These factors directly impact both gum disease treatment success and dental implant integration.
Diabetes and Dental Implant Success
Diabetes significantly impacts dental implant success rates when blood sugar levels are poorly controlled. High glucose levels interfere with the process of osseointegration, where the implant fuses with your jawbone. This critical phase determines whether your implant will provide stable, long-term tooth replacement.
Research shows that diabetic patients with poor glucose control experience higher rates of implant failure, delayed healing, and increased risk of peri-implantitis (infection around implants). However, diabetic patients with excellent blood sugar control can achieve implant success rates similar to non-diabetic patients when proper protocols are followed.
The timing of implant placement becomes crucial for diabetic patients. We often recommend stabilizing blood sugar levels and treating any existing gum disease before proceeding with dental implant treatment. This preparation phase may take several months but significantly improves long-term outcomes.
Risk Factors and Complications
Several diabetes-related factors increase implant complications beyond blood sugar control. Diabetic patients often experience slower wound healing, increased susceptibility to infections, and reduced bone quality around implant sites. Certain diabetes medications can also affect bone metabolism and healing capacity.
Advanced planning becomes essential for diabetic implant candidates. We may recommend:
- Pre-surgical blood sugar optimization
- Antibiotic prophylaxis protocols
- Modified healing timelines
- Enhanced follow-up schedules
- Specialized oral hygiene protocols
Prevention and Management Strategies
Excellent oral hygiene becomes even more critical for diabetic patients. Regular professional cleanings, typically every three to four months, help control bacterial levels and prevent gum disease progression. We often recommend antimicrobial rinses and specialized cleaning techniques for diabetic patients.
Close coordination with your physician ensures optimal diabetes management during dental treatment. We work with your medical team to time procedures when blood sugar levels are most stable and adjust treatment protocols based on your current diabetes control status.
Regular monitoring allows us to detect problems early and adjust treatment plans as needed. Diabetic patients benefit from more frequent periodontal evaluations and professional maintenance visits to prevent complications before they develop.
Choose Laudenbach Periodontics for Diabetic Dental Care
Managing both diabetes and oral health requires specialized knowledge and careful coordination between your medical and dental care teams. Our Philadelphia practice has extensive experience treating diabetic patients, understanding how to modify treatment protocols for optimal outcomes while maintaining your overall health and safety. We work closely with your physician to ensure your diabetes management supports successful periodontal treatment and implant therapy. Dr. Jay Laudenbach and our team provide comprehensive care tailored to your unique medical needs, helping you achieve the healthy smile you deserve despite the challenges diabetes may present. Don’t let diabetes prevent you from pursuing the periodontal care or dental implants you need. Contact our office to schedule a consultation and learn how we can help you achieve optimal oral health while managing your diabetes effectively.